What is a pneumothorax?
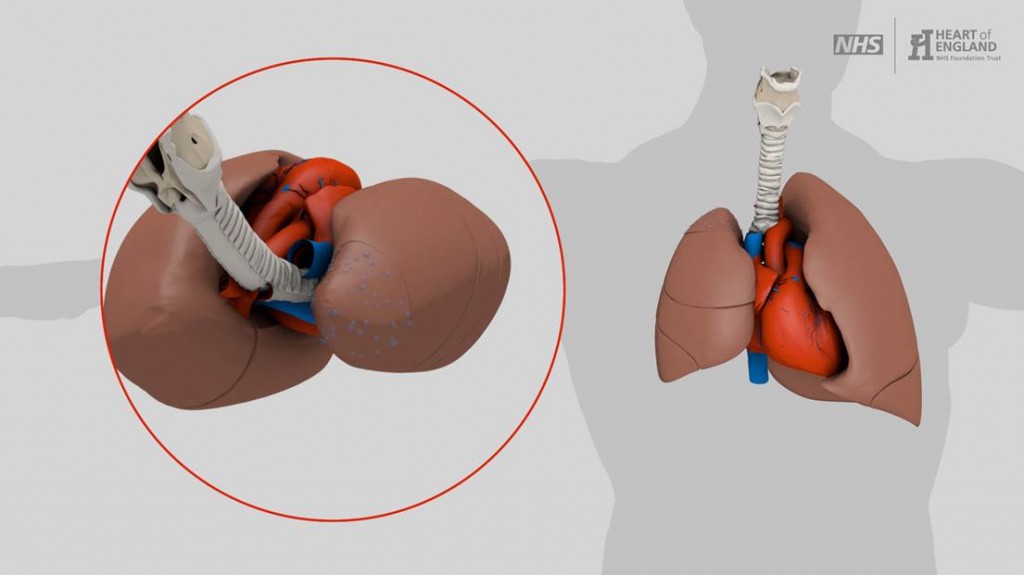
When air leaks out of the lung it collapses and leaves a space around it. The medical term for a collapsed lung is a pneumothorax. A small pneumothorax will often heal by itself, however sometimes they don’t heal up or they come back. A chest drain may be used at first but if this fails an operation may be needed to help re-inflate the lung and stop it collapsing again. If you have had a pneumothorax more than once, surgery is intended to help prevent this happening again.
Thoracic surgeons look after patients who need surgery for a pneumothorax. They also look after patients who have a pneumothorax that is difficult to treat, even if they do not need surgery.
- Trauma – including some medical procedures. Surgery is rarely required in this instance and the risk of it happening again without trauma are low.
- Lung diseases
- Smoking
- Young tall men are more at risk
- Young women may get a pneumothorax in relation to their menstrual cycle (catamenial pneumothorax)
 A number of techniques can be used to fix a pneumothorax. There are two parts to the surgery; dealing with area of lung that has leaked and preventing the pneumothorax from coming back. These procedures are done as keyhole (VATS) surgery. VATS stands for Video Assisted Thoracoscopic Surgery.
A number of techniques can be used to fix a pneumothorax. There are two parts to the surgery; dealing with area of lung that has leaked and preventing the pneumothorax from coming back. These procedures are done as keyhole (VATS) surgery. VATS stands for Video Assisted Thoracoscopic Surgery.
During surgery you lie on your side with your arm raised. Up to 4 small cuts are made, each about 5cm (2 in) long. These are used for the instruments and small camera to go into the chest. Special staples are used to cut and seal any parts of lung that need to be removed. The piece of lung can be removed through one of the small cuts. The wound is closed with dissolvable stitches. 1 or 2 chest drains are put in at the end of the operation and held in placed with a stitch. These remove any fluid or air from around the lung.
If a part of the operation cannot be done keyhole the operation may need to be changed to the open technique (thoracotomy). Open surgery is done with one longer cut under the shoulder blade between 2 ribs. The 2 ribs are parted to get into the chest. One rib may be cut to give more space, ribs are not removed. At the end of surgery the 2 ribs are held back together with strong stitches. The muscles and skin are also stitched back together.
If you have had repeated episodes of pneumothorax or you wish to do scuba diving your surgeon may decide it is best to use the open technique to do your operation.
- Dealing with area of lung that has leaked
Bubbles of thin lung tissue around the edge of the lung can be the cause of a pneumothorax if they burst. A small bubble is called a bleb, a large bubble is called a bulla. Removing these abnormal parts of the lung helps stop air leaking out of the lung. Removing such a small amount of lung does not give you any long term breathing problems.
- Preventing the pneumothorax from recurring
If the lung becomes stuck to the inside of the chest wall there is less chance of the lung collapsing. Removing the pleura on the inside of the ribs makes the inside of the chest wall sticky. This causes the lung to stick to chest wall. Alternatively sterile talc powder can be put into the chest usually during the operation. The powder causes irritation which makes the lung stick to the chest wall. The lung sticking to the chest wall is called pleurodesis.
Women affected by catamenial pneumothorax may benefit from hormonal treatment to stop ovulation. This is usually directed by a gynaecologist.
Particular care should be taken if you are considering flying or scuba diving.
- Flying
You must have had a chest X ray which shows the pneumothorax has completely gone. You must then wait at least 1 week after the chest X ray showing your pneumothorax has completely gone before flying. If you had a pneumothorax because of trauma, you must wait at least 2 weeks after the chest X ray showing your pneumothorax has completely gone before flying. Guidelines may change, you should check with your doctor before flying.
- Scuba diving
Diving without treatment for a pneumothorax is extremely dangerous. Diving causes big changes in the respiratory system and compression of air within the body. If your pneumothorax happened for no reason you should not dive unless you have had surgery on both sides of the chest to prevent a further pneumothorax. After surgery you will need to have normal lung function tests and a normal CT scan of the chest before diving. Guidelines may change. You should have a specialist assessment of your individual fitness for diving prior to doing so. Ask your diving organisation for contact details, some GPs may be able to do assessments but many of them will not have had the training to do so.
See also:
Pain control
Exercise and physiotherapy
In addition the following risks apply:
- Recurrence
If you had no specific cause of the pneumothorax, the risk of it coming back without surgery is 20 to 30 in 60. If the pneumothorax was caused by lung disease the risk of it coming back is 24 in 60. If you have VATS surgery pneumothorax, the risk of it coming back is 3 in 60 people.
Recurrence usually happens within a few years of the first pneumothorax but it can happen many years later. It may come back on the other side of the chest.
- Prolonged air leak
Air may continue to leak out of the lung after surgery. Occasionally this lasts for longer, possibly weeks. A chest drain will need to be in place until this settles, you may be able to go home with the chest drain still in and come back for regular check-ups until the air leak settles. The risk of this is higher if lung disease caused the pneumothorax.
If you do not want an operation other options may include:
- Continued use of chest drains.
Given enough time the lung should heal and stop leaking air, this may take weeks. If you have a lung disease and surgery would be too risky your surgeon may advise you it is safest to wait for the lung to heal. Different types of drains and drain settings may be used to try and help this process.
- Talc pleurodesis
We can help the lung stick to the chest wall without an operation in some cases. Sterile talc powder is mixed with sterile water and flushed up the chest drain. A small amount of your own blood may also be used instead of the talc and water mixture. This requires a chest drain but does not require you to be asleep under a general anaesthetic. Putting the talc powder in during an operation has a higher success rate than via a drain (95% for surgery vs 75% using the drain).